Physician-Led Anesthesia Care Provides Unique Value
As medical doctors, anesthesiologists keep patients safe, improve outcomes, protect your institution’s financial health, and increase the efficiency and quality of care across many medical and surgical specialties. They deliver unique value throughout the perioperative period.
New: Addressing workforce challenges
Doing more with less has become a reality for many hospitals and health systems. Your institution—big or small—is likely dealing with workforce issues, as a shortage of health care professionals coincides with an increased demand for their services, particularly for surgeries and advanced medical procedures.
Anesthesiologists are identifying short- and long-term solutions to continue serving your communities and uphold high-quality care while generating revenue and effectively managing resources.
AHA and ASA identify solutions for surgical backlogs. The American Hospital Association is working with the American Society of Anesthesiologists to share how health care leaders are relying on anesthesiologists to improve perioperative performance, expand the use of existing OR capacity, and explore new practice models to tackle the surgical backlog. Download a summary of their findings and listen to a related podcast:
Improving institutional performance
Removing anesthesiologists from anesthesia care is risky for your hospital and patients. You can partner with your anesthesiologists to reduce risk and enhance your hospital’s ratings and reputation.

Protecting your institution and patients with medical expertise
Anesthesiologists lead anesthesia care and provide an unparalleled level of education and training to protect patients.
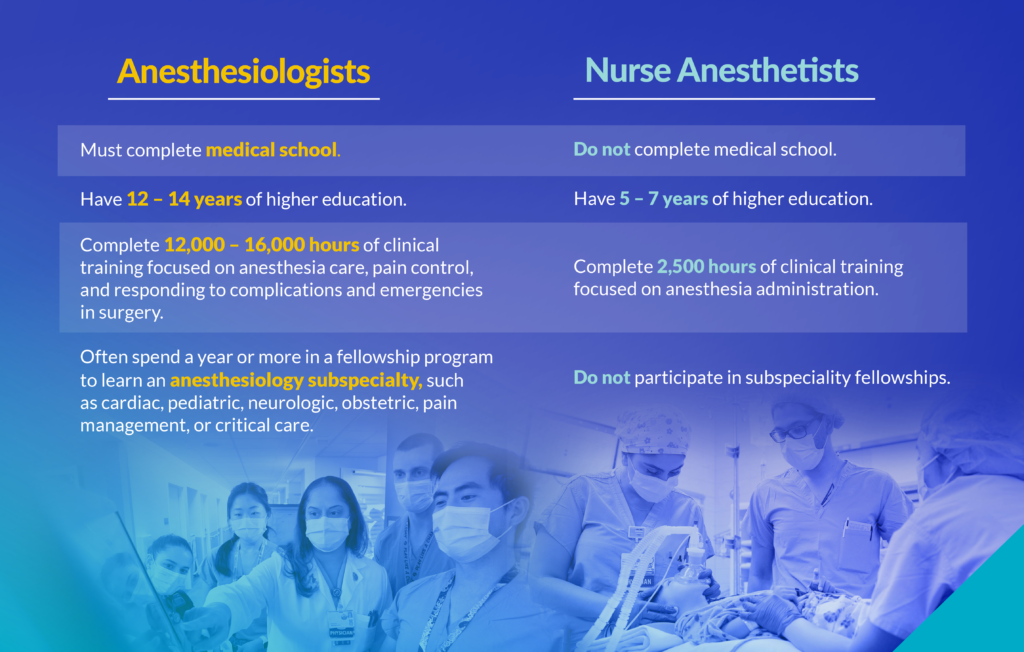
With specialized training, anesthesiologists identify and mitigate patient risk before surgery, prevent and respond to emergencies during surgery, and enhance postoperative recovery. They assume overall responsibility for anesthesia care while delegating appropriate roles to nonphysician anesthesia practitioners.
Anesthesiologists Improve Your Bottom Line
While hospitals and health care systems look to reduce costs, safety and quality cannot be overlooked. As essential providers on the Anesthesia Care Team, anesthesiologists can help control costs and maximize your institution’s financial health. Their years of training and work across medical departments enable them to identify efficiencies, conserve staffing resources, and generate revenue—all of which strengthen your financial performance.
Controlling costs during patient care
Research shows that anesthesiologists’ involvement in patient care helps control costs before, during, and after surgery by:
- Reducing unnecessary testing, same-day cancellations, operating room emergencies, and surgical complications.
- Decreasing the need for additional consults from other specialty physicians for services that could have been provided by an anesthesiologist.
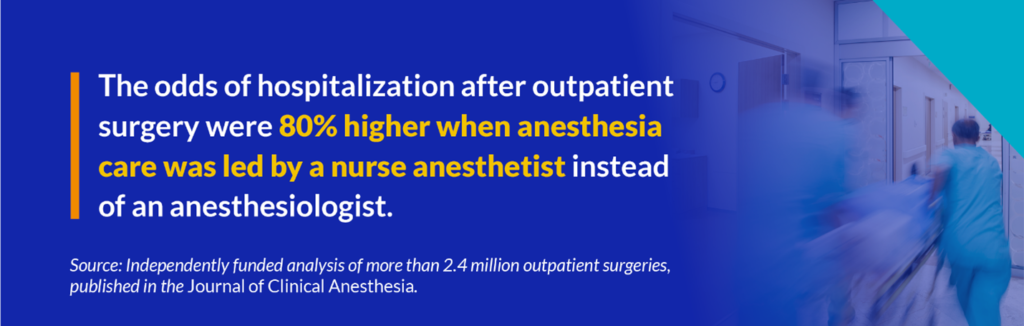
- Reducing the risk of hospitalization following outpatient surgery.
Learn more about anesthesiologists’ impact on costs.
Bolstering revenue and improving outcomes
Anesthesiologists identify and evaluate operating room efficiencies—improving first case on-time starts, operating room turnover times, post-anesthesia care unit discharge times, and more.
“We are in a position to drive value throughout the entire perioperative process, across a variety of surgical specialties, to ensure the best possible outcomes for patients at the most reasonable cost to the institution.”
— Steven Schulman, MD, MHA, FASA, Associate Medical Director
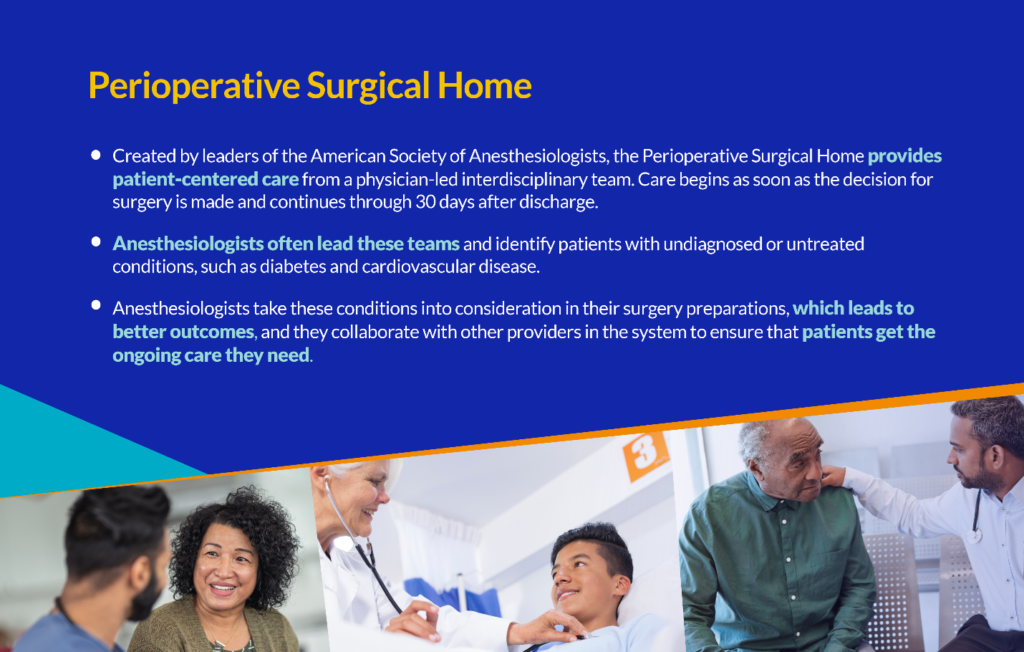
Programs developed and led by anesthesiologists, such as the Perioperative Surgical Home and Enhanced Recovery After Surgery, significantly reduce patient mortality and improve operating room efficiency.
Anesthesiologists Improve Health and Access to High-Quality Care for All Patients
Anesthesiologists play a critical role in perioperative care, maternal care, and pain management—areas that often see gaps in the quality of patient outcomes that are associated with race, geography, and other social factors.
Narrowing equity gaps in health care
Many medical conditions and complications disproportionately affect certain populations, such as historically marginalized racial and ethnic groups and those with low incomes. Often, these disparities arise from insufficient access to health care, which can leave medical conditions undetected or untreated. Anesthesiologists are well positioned to mitigate the consequences of unequal access to diagnosis and care because of their involvement with patients before and after surgery, which gives them the opportunity to identify and treat these conditions.
Safeguarding maternal health for marginalized patients
Anesthesiologists can play a role in mitigating the consequences of unequal access to maternal health care. As health care leaders know, maternal mortality rates are higher among low-income and minority populations, especially among Black women. Obstetric anesthesiologists work to prevent maternal deaths from cardiovascular disease, embolic disease, preeclampsia, postpartum hemorrhage, sepsis, and other conditions.