Opioid Abuse
Opioids are highly addictive, and opioid abuse has become a national crisis in the United States. Statistics highlight the severity of the epidemic, with the National Institute on Drug Abuse reporting that more than 2 million Americans abuse opioids and that more than 90 Americans die by opioid overdose every day, on average.
Why do people become addicted to opioids?
Opioids can make your brain and body believe the drug is necessary for survival. As you learn to tolerate the dose you’ve been prescribed,
How can you avoid addiction to opioids?
If you or a loved one is considering taking opioids to manage pain, it is vital to talk to an anesthesiologist or other pain medicine specialist about using them safely and exploring alternative options if needed. Learn how to work with your anesthesiologist or another physician to use opioids more wisely and safely and explore what pain management alternatives might work for you.

What are the signs of an addiction?
People addicted to drugs may change their behavior. Possible signs include:
- Mixing with different groups of people or changing friends
- Spending time alone and avoiding time with family and friends
- Losing interest in activities
- Not bathing, changing clothes, or brushing their teeth
- Being very tired and sad
- Eating more or less than usual
- Being overly energetic, talking fast, and saying things that don’t make sense
- Being nervous or cranky
- Quickly changing moods
- Sleeping at odd hours
- Missing important appointments
- Getting into trouble with the law
- Attending work or school on an erratic schedule
- Experiencing financial hardship
What should you do if you or someone you know is addicted?
If you or a loved one is ready to seek help for an addiction, the first step is to find a physician or other health professional who can help. Ask your physician for a referral to a medical professional in addiction medicine. Or search the American Society of Addiction Medicine’s website for addiction specialists in your area. The American Academy of Addiction Psychiatry also has a Patient Referral Program.
Another resource is the Substance Abuse and Mental Health Services Administration (SAMHSA) toll-free help line to find drug treatment near you: 1-800-662-HELP (4357). Or you can visit SAHMSA’s Behavioral Health Treatment Services Locator. There’s also a State Agencies webpage that helps you find state agencies that might have special programs for you or a loved one.
If you or a loved one is ready to seek assistance for an addiction, the first step is to find a physician or other health professional who can help.
If you are supporting a friend or loved one in overcoming addiction, the National Institute on Drug Abuse offers the following advice: Assure your friend or loved one that addiction can be managed successfully, but acknowledge that it may take several attempts at treatment to find the best approach. If your friend or loved one refuses to seek help, a confrontational “intervention” is not recommended. These encounters can escalate into violence or backfire in other ways. Try to convince the person to consult with a physician.
What are opioid withdrawal symptoms and how can you alleviate them?
Opioid withdrawal symptoms can but won’t necessarily include some of the following:
- Drug cravings
- Anxiety/irritability
- Insomnia
- Abdominal pain
- Vomiting
- Diarrhea
- Tremors (shaking)
- Feeling cold
Opioid withdrawal symptoms generally last between three and five days, although they can last up to 10 days, according to the American Society of Addiction Medicine (ASAM).
Withdrawal from opioids can be difficult and even dangerous. Trying to quit “cold turkey” is not recommended, ASAM advises, because it can lead to stronger cravings and continued use. The safest way to alleviate opioid withdrawal symptoms is through medically supervised treatment that generally includes medicines, counseling, and support. Some medications used to relieve withdrawal symptoms are methadone and buprenorphine (Subutex). These medications can also be used as long-term maintenance medicine for opioid dependence. In addition, a medication called clonidine can be used during withdrawal to help reduce anxiety, agitation, muscle aches, sweating, runny nose, and cramping. It does not help reduce cravings. The addiction medicine physician may also prescribe medication to treat vomiting and diarrhea and help with insomnia.
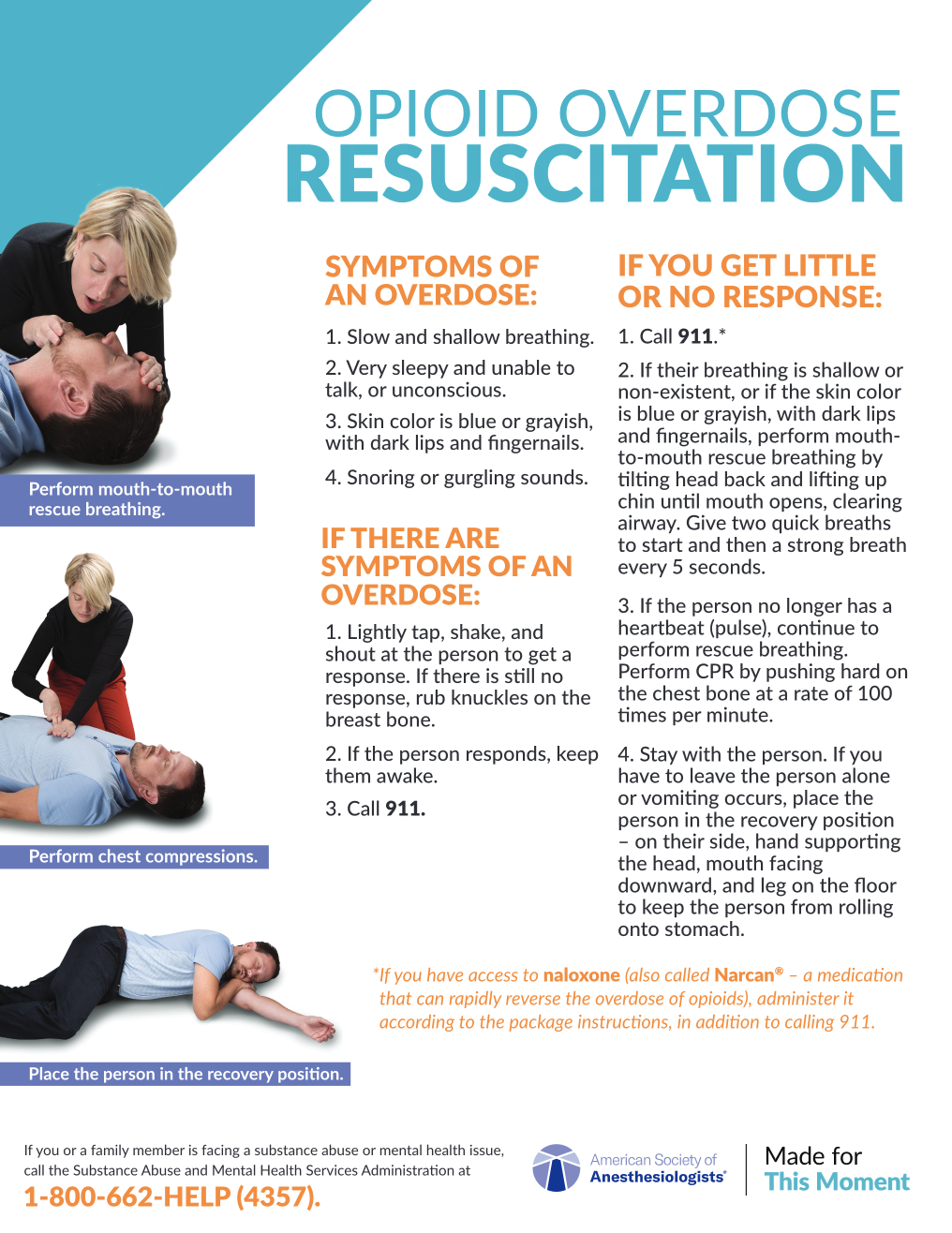
What are the symptoms of an opioid overdose?
Signs of an overdose include:
- Slow, shallow breathing
- Extreme sleepiness
- Inability to talk
- Blue skin color and dark-colored lips
- Snoring or gurgling sounds
How should you respond to an opioid overdose?
If you think someone may be experiencing an opioid overdose, take the following actions immediately:
- Lightly tap, shake, and shout at the person to get a response. If you do not get a response, rub your knuckles on the person’s breastbone.
- If the individual responds, keep the person awake.
- Call 911.
If You Get Little or No Response
If lightly tapping, shaking, and shouting at the person or rubbing your knuckles on the person’s breastbone do not elicit a response (per Step 1 above), take the following actions:
- Call 911. If you have naloxone, a medication that can rapidly reverse the effects of an overdose, administer it according to the instructions on the package (in addition to calling 911).
- If breathing is shallow or nonexistent, or if the person’s skin color is blue and he or she has dark-colored lips, perform mouth-to-mouth rescue breathing by tilting the head back and lifting up the chin until the mouth opens, clearing the airway. Give two quick breaths to start and then a strong breath every 5 seconds.
- If the person does not have a pulse or is not breathing, perform CPR. Push down repeatedly on the chest at a rate of 100 times per minute. Deliver rescue breaths after every 30 compressions.
- While waiting for emergency responders, stay with the person. If you must leave the person alone or vomiting occurs, place the individual in recovery position — on the person’s side, with the opposite hand supporting the head, mouth facing to the side and down, and top leg on the floor to keep the person from rolling onto the stomach.
What is naloxone and how can it help with an overdose?
Available as an injection or nasal spray, naloxone (also sold under the brand name Narcan) is a lifesaving medication that can rapidly reverse the effects of an opioid overdose. If you happen to have naloxone when responding to an overdose, call 911 and administer the medication according to the package instructions.
Access to naloxone is expanding on a state-by-state basis. It can be prescribed by a physician, is often carried by police officers and emergency medical responders, and is increasingly available over the counter at some pharmacies.
How should you store and dispose of opioids to protect family members?
If you are taking opioids, you are not the only one in your household who is in danger of misuse, addiction, and overdose. Other members of your household, including children, are also vulnerable. Here’s how to protect them:
- Always store opioids in a safe and secure place. Do not leave prescription bottles in the medicine cabinet, and keep the medication away from others, particularly young children. Children sometimes confuse medications with candy and end up swallowing them, which can lead to overdose. Other family members and visitors could also find prescription medications in the house and use them inappropriately.
- Never share your prescriptions. More than half of people who misuse prescribed opioids get them from a friend or relative, according to the Substance Abuse and Mental Health Services Administration.
- Don’t throw unused opioids in the trash. Improper disposal of prescription medicines can lead to other people finding and taking them.
If you have leftover or expired prescription medications, follow these drug disposal tips:
- Remove the prescription label that contains your name and other identifying information.
- Check with your municipal trash and recycling program providers about approved disposal drop-off options in your community, such as police stations.
- Look for pharmacies and health care clinics that provide drop-off boxes or sell specially designed drug disposal envelopes that you can seal and mail to an approved facility.
- Flush the medication down the toilet or mix it with dirt, kitty litter, or coffee grounds before throwing it in the garbage.